- Record: found
- Abstract: found
- Article: found
Update: Characteristics of Health Care Personnel with COVID-19 — United States, February 12–July 16, 2020
research-article
Michelle M. Hughes , PhD
1
,
,
Matthew R. Groenewold , PhD
1 ,
Sarah E. Lessem , PhD
1 ,
Kerui Xu , PhD
1 ,
Emily N. Ussery , PhD
1 ,
Ryan E. Wiegand , MS
1 ,
Xiaoting Qin , PhD
1 ,
Tuyen Do
1 ,
Deepam Thomas , MPH
2 ,
Stella Tsai , PhD
2 ,
Alexander Davidson , MPH
3 ,
Julia Latash , MPH
3 ,
Seth Eckel , MPH
4 ,
Jim Collins , MPH
4 ,
Mojisola Ojo , MPH
2 ,
Lisa McHugh , PhD
2 ,
Wenhui Li , PhD
3 ,
Judy Chen
3 ,
Jonathan Chan
3 ,
Jonathan M. Wortham , MD
1 ,
Sarah Reagan-Steiner , MD
1 ,
James T. Lee , MD
1 ,
Sujan C. Reddy , MD
1 ,
David T. Kuhar , MD
1 ,
Sherry L. Burrer , DVM
1 ,
Matthew J. Stuckey , PhD
1
25 September 2020
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
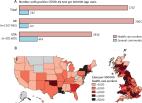
As of September 21, 2020, the coronavirus disease 2019 (COVID-19) pandemic had resulted
in 6,786,352 cases and 199,024 deaths in the United States.* Health care personnel
(HCP) are essential workers at risk for exposure to patients or infectious materials
(
1
). The impact of COVID-19 on U.S. HCP was first described using national case surveillance
data in April 2020 (
2
). Since then, the number of reported HCP with COVID-19 has increased tenfold. This
update describes demographic characteristics, underlying medical conditions, hospitalizations,
and intensive care unit (ICU) admissions, stratified by vital status, among 100,570
HCP with COVID-19 reported to CDC during February 12–July 16, 2020. HCP occupation
type and job setting are newly reported. HCP status was available for 571,708 (22%)
of 2,633,585 cases reported to CDC. Most HCP with COVID-19 were female (79%), aged
16–44 years (57%), not hospitalized (92%), and lacked all 10 underlying medical conditions
specified on the case report form
†
(56%). Of HCP with COVID-19, 641 died. Compared with nonfatal COVID-19 HCP cases,
a higher percentage of fatal cases occurred in males (38% versus 22%), persons aged
≥65 years (44% versus 4%), non-Hispanic Asians (Asians) (20% versus 9%), non-Hispanic
Blacks (Blacks) (32% versus 25%), and persons with any of the 10 underlying medical
conditions specified on the case report form (92% versus 41%). From a subset of jurisdictions
reporting occupation type or job setting for HCP with COVID-19, nurses were the most
frequently identified single occupation type (30%), and nursing and residential care
facilities were the most common job setting (67%). Ensuring access to personal protective
equipment (PPE) and training, and practices such as universal use of face masks at
work, wearing masks in the community, and observing social distancing remain critical
strategies to protect HCP and those they serve.
Data from laboratory-confirmed and probable COVID-19 cases, voluntarily reported to
CDC from state, local, and territorial health departments during February 12–July
16, 2020, were analyzed. COVID-19 cases are reported using a standardized case report
form, which collects information on demographic characteristics, whether the case
occurred in a U.S. health care worker (HCP status), symptom onset date, underlying
medical conditions, hospitalization, ICU admission, and death. HCP occupation type
and job setting were added to the case report form in May, enabling prospective and
retrospective entry of these elements. Case surveillance data were enriched with additional
cases from a COVID-19 mortality-focused supplementary surveillance effort in three
jurisdictions
§
(
3
). Descriptive analyses were used to examine characteristics by vital status. HCP
occupation type and job setting were reported by a subset of jurisdictions with at
least five HCP cases for each variable. Analyses were conducted using Stata (version
15.1; StataCorp) and SAS (version 9.4; SAS Institute).
Among 2,633,585 U.S. COVID-19 cases reported individually to CDC during February 12–July
16, HCP status was available for 571,708 (22%) persons, among whom 100,481 (18%) were
identified as HCP. Data completeness for HCP status varied by jurisdiction; among
jurisdictions that included HCP status on ≥70% of cases and reported at least one
HCP case (11), HCP accounted for 14% (14,938 of 109,293) of cases with HCP status
available and 11% (14,938 of 132,340) of all reported cases. Case report form data
were enriched with 89 additional HCP cases using supplementary mortality data; thus,
the final HCP case total for analysis was 100,570 (Table 1).
TABLE 1
Demographics, underlying medical conditions, hospitalization status, and intensive
care unit (ICU) status among health care personnel (HCP) with COVID-19, by vital status
— United States, February 12–July 16, 2020
Characteristic*
No. (%)
Case fatality ratio,§ no./total no.
Total
Alive
Deceased†
Unknown
Total
100,570
67,105
641
32,824
0.95 (641/67,746)
Age group (yrs)
N = 100,432
N = 67,023
N = 641
N = 32,768
—
16–44
57,742 (57)
39,018 (58)
57 (9)
18,667 (57)
0.15 (57/39,075)
45–54
20,981 (21)
13,836 (21)
99 (15)
7,046 (22)
0.71 (99/13,935)
55–64
17,052 (17)
11,264 (17)
205 (32)
5,583 (17)
1.79 (205/11,469)
≥65
4,657 (5)
2,905 (4)
280 (44)
1,472 (4)
8.79 (280/3,185)
Sex
N = 99,741
N = 66,796
N = 639
N = 32,306
—
Female
78,328 (79)
52,366 (78)
395 (62)
25,567 (79)
0.75 (395/52,761)
Male
21,413 (21)
14,430 (22)
244 (38)
6,739 (21)
1.66 (244/14,674)
Race/Ethnicity
N = 69,678
N = 45,104
N = 552
N = 24,022
—
American Indian/Alaska Native, non-Hispanic
253 (0)
186 (0)
0 (0)
67 (0)
—
Asian, non-Hispanic
6,010 (9)
4,083 (9)
111 (20)
1,816 (8)
2.65 (111/4,194)
Black, non-Hispanic
18,117 (26)
11,172 (25)
177 (32)
6,768 (28)
1.56 (177/11,349)
Hispanic/Latino¶
8,030 (12)
4,262 (9)
49 (9)
3,719 (15)
1.14 (49/4,311)
Multiple/Other, non-Hispanic
4,195 (6)
2,662 (6)
13 (2)
1,520 (6)
0.49 (13/2,675)
Native Hawaiian/Other Pacific Islander, non-Hispanic
422 (1)
314 (1)
4 (1)
104 (0)
1.26 (4/318)
White, non-Hispanic
32,651 (47)
22,425 (50)
198 (36)
10,028 (42)
0.88 (198/22,623)
Underlying medical conditions**
N = 40,582
N = 26,868
N = 378
N = 13,336
—
Any underlying medical condition
17,838 (44)
11,012 (41)
348 (92)
6,478 (49)
3.06 (348/11,360)
Any chronic lung disease
6,422 (16)
4,064 (15)
89 (24)
2,269 (17)
2.14 (89/4,153)
Any cardiovascular disease
7,348 (18)
4,331 (16)
229 (61)
2,788 (21)
5.02 (229/4,560)
Diabetes mellitus
5,466 (13)
3,314 (12)
198 (52)
1,954 (15)
5.64 (198/3,512)
Immunosuppressing condition
1,504 (4)
1,070 (4)
24 (6)
410 (3)
2.19 (24/1,094)
Severe obesity
1,101 (3)
453 (2)
27 (7)
621 (5)
5.63 (27/480)
Chronic renal disease
503 (1)
279 (1)
45 (12)
179 (1)
13.89 (45/324)
Neurologic/Neurodevelopmental disability
528 (1)
333 (1)
34 (9)
161 (1)
9.26 (34/367)
Chronic liver disease
242 (1)
148 (1)
10 (3)
84 (1)
6.33 (10/158)
Autoimmune condition
479 (1)
262 (1)
3 (1)
214 (2)
1.13 (3/265)
Psychologic/psychiatric condition
353 (1)
191 (1)
4 (1)
158 (1)
2.05 (4/195)
Admission to hospital
N = 83,202
N = 55,415
N = 591
N = 27,196
—
Yes
6,832 (8)
4,207 (8)
518 (88)
2,107 (8)
10.96 (518/4,725)
Admission to ICU
N = 33,694
N = 22,545
N = 377
N = 10,772
—
Yes
1,684 (5)
662 (3)
295 (78)
727 (7)
30.83 (295/957)
Abbreviation: COVID-19 = coronavirus disease 2019.
* Variable completeness varied by case characteristic: age (>99%), sex (99%), race
and ethnicity (69%), hospitalization status (83%), ICU admission status (34%); characteristic-specific
sample size for cases with available information are presented for each grouping.
N = number with available information.
† Death outcomes were known for 67,746 (67%) HCP cases; of these, 91 additional new
fatal cases were included based on data from the supplementary mortality project (89
newly identified as HCP and two newly identified deaths among known HCP). Additional
available data for these 91 cases were incorporated if missing in the national case
surveillance data.
§ Deaths per 100 HCP cases with known death status.
¶ Cases reported as Hispanic were categorized as “Hispanic or Latino persons of any
race” regardless of availability of race data.
** Underlying medical condition status was classified as “known” if any of these 10
conditions, specified on the standard case report form, were reported as present or
absent: diabetes mellitus, cardiovascular disease (includes hypertension), severe
obesity (body mass index ≥40 kg/m2), chronic renal disease, chronic liver disease,
chronic lung disease, immunosuppressing condition, autoimmune condition, neurologic
condition (including neurodevelopmental, intellectual, physical, visual, or health
impairment), or psychologic/psychiatric condition. Status for these conditions was
“known” for 40,582 persons. Responses include data from standardized fields supplemented
with data from the free text field for “other chronic disease/underlying condition”
for the 10 specific medical conditions, if not originally specified.
Among HCP with COVID-19 overall, the median age was 41 years (interquartile range = 30–53
years); 79% of cases were in females. Among 69,678 (69%) HCP cases with data on race
and ethnicity, 47% were in non-Hispanic Whites (Whites), 26% were in Blacks, 12% were
in Hispanics or Latinos of any race (Hispanics), and 9% were in Asians. Of persons
with known hospitalization or ICU admission status, 8% (6,832 of 83,202) were hospitalized
and 5% (1,684 of 33,694) were treated in an ICU. Vital status was known for 67% (67,746)
of HCP with COVID-19; among those, 641 (1%) died. Deaths among HCP with COVID-19 were
reported in 22 jurisdictions. Compared with those who survived, decedents tended to
be older (median age = 62 versus 40 years), male (38% versus 22%), Asian (20% versus
9%), or Black (32% versus 25%).
Among HCP cases with data on one or more of 10 underlying medical conditions specified
on the case report form, 17,838 (44%) persons had at least one condition. The most
common were cardiovascular disease (18%), chronic lung disease (16%), and diabetes
mellitus (13%). The vast majority (92%) of fatal HCP cases were among HCP with an
underlying medical condition. More than one half had cardiovascular disease (61%)
or diabetes mellitus (52%), conditions known to increase the risk for severe COVID-19
¶
; 32% were reported to have both conditions (Table 1).
Six jurisdictions reported the occupation type** or job setting
††
for at least five HCP with COVID-19 (Table 2). Among HCP with COVID-19 in these jurisdictions,
occupation type was available for 59% (5,913 of 9,984) and job setting for 41% (6,955
of 17,052). Health care support workers accounted for the largest overall group of
occupation types (32%), and nurses constituted the largest single occupation type
(30%) (Table 2). Within this subset of HCP cases, two thirds (67%) were in persons
reported to work in nursing and residential care facilities.
TABLE 2
Occupation type and job setting of health care personnel (HCP) with COVID-19 — six
jurisdictions,* February 12–July 16, 2020
Characteristic (no. with available information)†
No. (%)
Occupation type (5,913)§
Health care support worker¶
1,895 (32.1)
Nurse**
1,742 (29.5)
Administrative staff member
581 (9.8)
Environmental services worker
330 (5.6)
Physician
190 (3.2)
Medical technician
135 (2.3)
Behavioral health worker
128 (2.2)
First responder
113 (1.9)
Dietary services worker
113 (1.9)
Dental worker
98 (1.7)
Laboratorian
68 (1.2)
Occupational, physical, or speech therapist
65 (1.1)
Pharmacy worker
62 (1.1)
Respiratory therapist
44 (0.7)
Phlebotomist
25 (0.4)
Physician assistant
13 (0.2)
Other
311 (5.3)
Job setting (6,955)§
Nursing and residential care facility††,§§
4,649 (66.8)
Hospital
1,231 (17.7)
Ambulatory health care service¶¶
804 (11.6)
Other
271 (3.9)
Abbreviation: COVID-19 = coronavirus disease 2019.
* Alaska, Kansas, Michigan, Minnesota, North Carolina, and Utah.
† Occupation type data are included for five jurisdictions (Alaska, Kansas, Minnesota,
North Carolina, and Utah) that reported occupation type for at least five HCP COVID-19
cases; occupation type data were known for 59% (5,913 of 9,984) of HCP cases in those
jurisdictions. Job setting data are included for five jurisdictions (Alaska, Kansas,
Michigan, Minnesota, and Utah) that reported job setting for at least five HCP COVID-19
cases; job setting data were known for 41% (6,955 of 17,052) of HCP cases in those
jurisdictions.
§ Occupation type and job setting categories were determined either by inclusion on
the CDC case report form or by manual review and categorization of free-text entries
within “other, specify” fields. Free-text data were used to supplement existing categories
for occupation (nurse, environmental services worker, physician, respiratory therapist)
and setting (long-term care facility [including nursing home/assisted living facility],
hospital, rehabilitation facility) and create new categories.
¶ Includes nursing assistant (1,444), medical assistant (123), and other care provider
or aide (328); free-text fields were used to create new categories.
**Includes data from standardized fields (1,724) supplemented with data from free-text
fields (18); types of nurses or nursing specialties are not specified.
†† Includes long-term care facility (including nursing home/assisted living facility)
(4,424), rehabilitation facility (131), and group home (94).
§§ Michigan provides job setting data only for cases identified from long-term care
facilities (2,800).
¶¶ Includes outpatient care center (422), home health care service (317), and dental
facility (65); free-text fields were used to create new categories.
Discussion
State, local, and territorial health departments voluntarily submit COVID-19 case
notification data to CDC, and these critical data help provide a national picture
of cases. The first report on HCP with COVID-19 using national case surveillance data
in April 2020 (
2
) described characteristics of 9,282 HCP cases and 27 deaths among approximately 315,000
total cases. As of July 16, 2020, among approximately 2.5 million reported U.S. COVID-19
cases, 100,570 cases in HCP and 641 deaths among HCP with COVID-19 have been reported
to CDC. Continued national surveillance is vital to evaluate the effect of the pandemic
on HCP, and this update emphasizes the ongoing impact on this essential working population.
Among reported HCP with COVID-19, age and sex distributions remain comparable to those
of the overall U.S. HCP workforce
§§
; however, compared with nonfatal COVID-19 cases in HCP, fatal HCP cases were more
common among older persons and males. Similar to findings described in the overall
population (
4
,
5
), HCP with underlying medical conditions who developed COVID-19 were at increased
risk for death. Almost all reported HCP with COVID-19 who died had at least one of
10 underlying conditions listed on the case report form, compared with fewer than
one half of those who survived. Asian and Black HCP were also more prevalent among
fatal cases; disproportionate mortality of persons from some racial and ethnic groups
among cases has also been described in the general population (
3
). Long-standing inequities in social determinants of health can result in some groups
being at increased risk for illness and death from COVID-19, and these factors must
also be recognized and addressed when protecting essential workers in the workplace,
at home, and in the community. Ensuring adequate allocation of PPE to all HCP in the
workplace is one important approach to mitigating systemic inequalities in COVID-19
risk (
6
). As the COVID-19 pandemic continues in the United States, HCP are faced with increasing
fatigue, demands, and stressors. HCP who are at higher risk for severe illness and
death from COVID-19 should maintain ongoing communication with their personal health
care providers and occupational health services to manage their risks at work and
in the community.
In this update, most HCP with COVID-19 were reported to work in nursing and residential
care facilities. Large COVID-19 outbreaks in long-term care facilities suggest that
transmission occurs among residents and staff members (
7
,
8
). During the COVID-19 pandemic, multiple challenges in long-term care settings have
been identified, including inadequate staffing and PPE, and insufficient training
in infection prevention and control. As the pandemic continues, it is essential to
meet the health and safety needs of HCP serving populations requiring long-term care.
Importantly, HCP cases were also identified from a variety of other health care settings.
Therefore, increased access to resources, appropriate training, and ongoing support
are needed across the health care spectrum to protect all HCP and their patients.
HCP with COVID-19 were reported among a diverse range of occupations. Nurses represented
30% of HCP cases with known occupation type, but account for only approximately 15%
of the total U.S. health care and social assistance workforce.
¶¶
Nurses and health care support workers often have frequent, close contact with patients
and work in settings that might increase their risk for acquiring SARS-CoV-2, the
virus that causes COVID-19. HCP who do not provide direct patient care, such as administrative
staff members and environmental service workers, were also reported to have COVID-19.
Risk to HCP can occur through pathways other than direct patient care, such as exposure
to coworkers, household members, or persons in the community. HCP who acquire SARS-CoV-2
can similarly introduce the virus to patients, coworkers, or persons outside the workplace.
Thus, practices such as universal use of face masks at work, wearing masks in the
community, observing social distancing, and practicing good hand hygiene remain critical
strategies to protect HCP and the populations they serve. Screening HCP for illness
before workplace entry and providing nonpunitive sick leave options remain critical
practices.
The findings in this report are subject to at least five limitations. First, although
reporting completeness increased from 16% in April to 22% in July (
2
), HCP status remains missing for most cases reported to CDC. HCP might be prioritized
for testing, but the actual number of cases in this population is most certainly underreported
and underdetected, especially in asymptomatic persons (
9
,
10
). Second, the amount of missing data varied across demographic groups, underlying
medical conditions, and health outcomes; persons with known HCP status and other information
might differ systematically from those for whom this information is not available.
Third, details of HCP occupation type and job setting were not included on the CDC
case report form until May 2020, and only six jurisdictions reported these data. Fourth,
testing strategies and availability can vary by jurisdiction and health care setting,
influencing the numbers and types of HCP cases detected. Finally, this report does
not include information on whether exposure to SARS-CoV-2 among HCP cases occurred
in the workplace or in other settings, such as the household or community.
As of July 16, 2020, 100,570 COVID-19 cases in HCP and 641 deaths among HCP with COVID-19
were reported in the United States. Information on COVID-19 among essential workers,
including HCP, can inform strategies needed to protect these populations and those
they serve, including decisions related to COVID-19 vaccination, when available. Factors
such as demographics, including race and ethnicity, underlying health conditions,
occupation type, and job setting can contribute to the risk of HCP acquiring COVID-19
and experiencing severe outcomes, including death. Given the evidence of ongoing COVID-19
infections among HCP and the critical role these persons play in caring for others,
continued protection of this population at work, at home, and in the community remains
a national priority.***
Summary
What is already known about this topic?
Health care personnel (HCP) are essential workers at risk for COVID-19.
What is added by this report?
HCP with COVID-19 who died tended to be older, male, Asian, Black, and have an underlying
medical condition when compared with HCP who did not die. Nursing and residential
care facilities were the most commonly reported job setting and nursing the most common
single occupation type of HCP with COVID-19 in six jurisdictions.
What are the implications for public health practice?
Continued surveillance is vital to understand the impact of COVID-19 on essential
workers. Ensuring access to personal protective equipment and training, and practices
such as universal use of face masks at work, wearing masks in the community, and observing
social distancing remain critical strategies to protect HCP and those they serve.
Related collections
Most cited references9
- Record: found
- Abstract: found
- Article: not found
Presymptomatic SARS-CoV-2 Infections and Transmission in a Skilled Nursing Facility
Melissa M. Arons, Kelly Hatfield, Sujan Reddy … (2020)

- Record: found
- Abstract: found
- Article: found
Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 — COVID-NET, 14 States, March 1–30, 2020
Shikha Garg, Lindsay Kim, Michael Whitaker … (2020)
- Record: found
- Abstract: found
- Article: found
Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study
Long H Nguyen, David A Drew, Mark S. Graham … (2020)