- Record: found
- Abstract: found
- Article: found
The Effect of Air Tourniquet on Interleukin-6 Levels in Total Knee Arthroplasty
Read this article at
Abstract
Background:
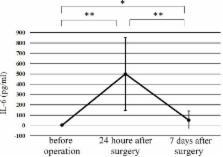
Air tourniquet-induced skeletal muscle injury increases the concentrations of some cytokines such as interleukin-6 (IL-6) in plasma. However, the effect of an air tourniquet on the IL-6 concentrations after total knee arthroplasty (TKA) is unclear. We therefore investigated the impact of tourniquet-induced ischemia and reperfusion injury in TKA using the IL-6 level as an index.
Methods:
Ten patients with primary knee osteoarthrosis who underwent unilateral TKA without an air tourniquet were recruited (Non-tourniquet group). We also selected 10 age- and sex-matched control patients who underwent unilateral TKA with an air tourniquet (Tourniquet group). Venous blood samples were obtained at 3 points; before surgery, 24 h after surgery, and 7 days after surgery.
The following factors were compared between the two groups; IL-6, C-reactive protein (CRP), creatine phosphokinase (CPK), the mean white blood cell (WBC) counts, and the maximum daily body temperatures.
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: not found
The pathophysiology of skeletal muscle ischemia and the reperfusion syndrome: a review.
- Record: found
- Abstract: found
- Article: not found
C-reactive protein (CRP) levels after elective orthopedic surgery.
- Record: found
- Abstract: found
- Article: not found