- Record: found
- Abstract: found
- Article: not found
Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Read this article at
ABSTRACT
The Dietary Approaches to Stop Hypertension (DASH) diet is recognized as an effective dietary intervention to reduce blood pressure (BP). However, among randomized controlled trials (RCTs) investigating the DASH diet–mediated BP reduction, there are significant methodological and clinical differences. The purpose of this study was to comprehensively assess the DASH diet effect on BP in adults with and without hypertension, accounting for underlying methodological and clinical confounders. We systematically searched Medline and the Cochrane Collaboration Library databases and identified 30 RCTs (n = 5545 participants) that investigated the BP effects of the DASH diet compared with a control diet in hypertensive and nonhypertensive adults. Both random-effects and fixed-effect models were used to calculate the mean attained systolic BP (SBP) and diastolic BP (DBP) differences during follow-up. Subgroup and meta-regression analyses were also conducted. Compared with a control diet, the DASH diet reduced both SBP and DBP (difference in means: −3.2 mm Hg; 95% CI: −4.2, −2.3 mm Hg; P < 0.001, and −2.5 mm Hg; 95% CI: −3.5, −1.5 mm Hg; P < 0.001, respectively). Hypertension status did not modify the effect on BP reduction. The DASH diet compared with a control diet reduced SBP levels to a higher extent in trials with sodium intake >2400 mg/d than in trials with sodium intake ≤2400 mg/d, whereas both SBP and DBP were reduced more in trials with mean age <50 y than in trials of older participants. The quality of evidence was rated as moderate for both outcomes according to the Grading of Recommendations, Assessment, Development, and Evaluation approach. The adoption of the DASH diet was accompanied by significant BP reduction in adults with and without hypertension, although higher daily sodium intake and younger age enhanced the BP-lowering effect of the intervention.
This meta-analysis was registered at www.crd.york.ac.uk/prospero as CRD42019128120.
Related collections
Most cited references58
- Record: found
- Abstract: found
- Article: found
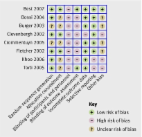
The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials
- Record: found
- Abstract: found
- Article: not found
Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement
- Record: found
- Abstract: found
- Article: found
