- Record: found
- Abstract: found
- Article: found
New Cancer Diagnoses Before and During the COVID-19 Pandemic

Read this article at
Key Points
Question
Is there an association between the COVID-19 pandemic and cancer incidence in Manitoba, Canada?
Findings
In this cross-sectional study including 48 378 individuals with cancer diagnoses, a significant decrease in cancer diagnosis incidence was observed in the first few months of the pandemic, particularly in breast, colon, and rectal cancer incidence. Other cancer sites showed minimal long-term changes in incidence.
Abstract
This cross-sectional study evaluates associations between the COVID-19 pandemic and cancer incidence in Manitoba, Canada.
Abstract
Importance
Disruptions to health care during the COVID-19 pandemic may have led to missed cancer diagnoses. It is critical to evaluate the association between the COVID-19 pandemic and cancer incidence to address public and patient anxiety, inform recovery efforts, and identify strategies to reduce the system’s vulnerability to future disruptions.
Objective
To examine the association between the COVID-19 pandemic and cancer incidence in Manitoba, Canada.
Design, Setting, and Participants
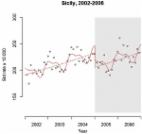
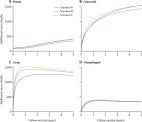
A population-based cross-sectional study design was conducted using data from the Manitoba Cancer Registry and an interrupted time-series analysis. All individuals diagnosed with cancer in Manitoba, Canada, from January 1, 2015, until December 31, 2021, were included. Individuals diagnosed with breast, colon, rectal, or lung cancer were grouped by age as follows: younger than 50 years, 50 to 74 years, and 75 years and older.
Main Outcomes and Measures
Age-standardized cancer incidence rates and the estimated cumulative difference between the number of cases in the absence of COVID-19 and observed (fitted) number of cancer cases.
Results
A total of 48 378 individuals were included. The median (IQR) age at diagnosis was 68 (59-77) years and 23 972 participants (49.6%) were female. In April 2020, there was a 23% decrease in overall cancer incidence. Cancer incidence decreased by 46% for breast, 35% for colon, 47% for rectal, 50% for head and neck, 65% for melanoma, and 33% for endocrine cancer diagnoses and increased by 12% for hematological cancer diagnoses and 8% for diagnoses of cancers with an unknown primary site. Lung cancer incidence remained stable until December 2020 when it decreased by 11%. Brain and central nervous system and urinary cancer diagnoses decreased consistently over time from April 2020 to December 2021 by 26% and 12%, respectively. No association was observed with gynecologic (1% increase), other digestive (1% decrease), or pancreatic (7% increase) cancer incidence. As of December 2021, Manitoba had an estimated deficit of 692 (5.3%) cancers. The largest estimated deficits were for breast (273 cases, 14.1% deficit), colon (133 cases, 12.2% deficit), and lung cancers (132 cases, 7.6% deficit).
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: found
Interrupted time series regression for the evaluation of public health interventions: a tutorial
- Record: found
- Abstract: found
- Article: found
The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study

- Record: found
- Abstract: found
- Article: found