- Record: found
- Abstract: found
- Article: not found
Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks
Abstract
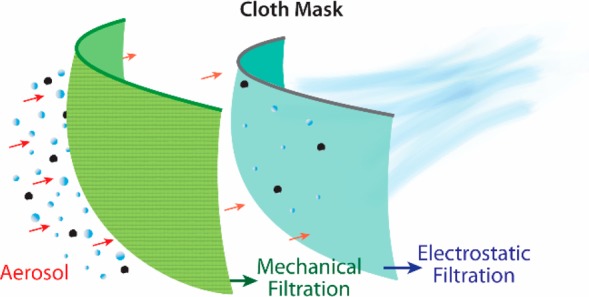
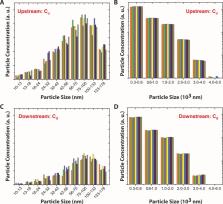
The emergence of a pandemic affecting the respiratory system can result in a significant demand for face masks. This includes the use of cloth masks by large sections of the public, as can be seen during the current global spread of COVID-19. However, there is limited knowledge available on the performance of various commonly available fabrics used in cloth masks. Importantly, there is a need to evaluate filtration efficiencies as a function of aerosol particulate sizes in the 10 nm to 10 μm range, which is particularly relevant for respiratory virus transmission. We have carried out these studies for several common fabrics including cotton, silk, chiffon, flannel, various synthetics, and their combinations. Although the filtration efficiencies for various fabrics when a single layer was used ranged from 5 to 80% and 5 to 95% for particle sizes of <300 nm and >300 nm, respectively, the efficiencies improved when multiple layers were used and when using a specific combination of different fabrics. Filtration efficiencies of the hybrids (such as cotton–silk, cotton–chiffon, cotton–flannel) was >80% (for particles <300 nm) and >90% (for particles >300 nm). We speculate that the enhanced performance of the hybrids is likely due to the combined effect of mechanical and electrostatic-based filtration. Cotton, the most widely used material for cloth masks performs better at higher weave densities ( i.e., thread count) and can make a significant difference in filtration efficiencies. Our studies also imply that gaps (as caused by an improper fit of the mask) can result in over a 60% decrease in the filtration efficiency, implying the need for future cloth mask design studies to take into account issues of “fit” and leakage, while allowing the exhaled air to vent efficiently. Overall, we find that combinations of various commonly available fabrics used in cloth masks can potentially provide significant protection against the transmission of aerosol particles.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1
- Record: found
- Abstract: found
- Article: not found
Respiratory virus shedding in exhaled breath and efficacy of face masks
- Record: found
- Abstract: found
- Article: not found
Airborne transmission of SARS-CoV-2: the world should face the reality
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.