- Record: found
- Abstract: found
- Article: found
Who pays for healthcare in Bangladesh? An analysis of progressivity in health systems financing
Read this article at
Abstract
Background
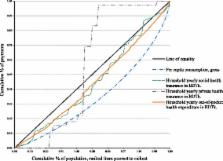
The relationship between payments towards healthcare and ability to pay is a measure of financial fairness. Analysis of progressivity is important from an equity perspective as well as for macroeconomic and political analysis of healthcare systems. Bangladesh health systems financing is characterized by high out-of-pocket payments (63.3%), which is increasing. Hence, we aimed to see who pays what part of this high out-of-pocket expenditure. To our knowledge, this was the first progressivity analysis of health systems financing in Bangladesh.
Methods
We used data from Bangladesh Household Income and Expenditure Survey, 2010. This was a cross sectional and nationally representative sample of 12,240 households consisting of 55,580 individuals. For quantification of progressivity, we adopted the ‘ability-to-pay’ principle developed by O’Donnell, van Doorslaer, Wagstaff, and Lindelow (2008). We used the Kakwani index to measure the magnitude of progressivity.
Results
Health systems financing in Bangladesh is regressive. Inequality increases due to healthcare payments. The differences between the Gini coefficient and the Kakwani index for all sources of finance are negative, which indicates regressivity, and that financing is more concentrated among the poor. Income inequality increases due to high out-of-pocket payments. The increase in income inequality caused by out-of-pocket payments is 89% due to negative vertical effect and 11% due to horizontal inequity.
Conclusions
Our findings add substantial evidence of health systems financing impact on inequitable financial burden of healthcare and income. The heavy reliance on out-of-pocket payments may affect household living standards. If the government and people of Bangladesh are concerned about equitable financing burden, our study suggests that Bangladesh needs to reform the health systems financing scheme.
Related collections
Most cited references22
- Record: found
- Abstract: not found
- Article: not found
Measurement of Tax Progressivity: An International Comparison
- Record: found
- Abstract: found
- Article: not found
Insuring Consumption Against Illness

- Record: found
- Abstract: found
- Article: found