- Record: found
- Abstract: found
- Article: found
Temocillin versus meropenem for the targeted treatment of bacteraemia due to third-generation cephalosporin-resistant Enterobacterales (ASTARTÉ): protocol for a randomised, pragmatic trial
Read this article at
Abstract
Introduction
Alternatives to carbapenems are needed in the treatment of third-generation cephalosporin-resistant Enterobacterales (3GCR-E). Temocillin is a suitable candidate, but comparative randomised studies are lacking. The objective is to investigate if temocillin is non-inferior to carbapenems in the targeted treatment of bacteraemia due to 3GCR-E.
Methods and analysis
Multicentre, open-label, randomised, controlled, pragmatic phase 3 trial. Patients with bacteraemia due to 3GCR-E will be randomised to receive intravenously temocillin (2 g three times a day) or carbapenem (meropenem 1 g three times a day or ertapenem 1 g once daily). The primary endpoint will be clinical success 7–10 days after end of treatment with no recurrence or death at day 28. Adverse events will be collected; serum levels of temocillin will be investigated in a subset of patients. For a 10% non-inferiority margin, 334 patients will be included (167 in each study arm). For the primary analysis, the absolute difference with one-sided 95% CI in the proportion of patients reaching the primary endpoint will be compared in the modified intention-to-treat population.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: found
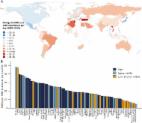
Global increase and geographic convergence in antibiotic consumption between 2000 and 2015

Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.