- Record: found
- Abstract: found
- Article: found
Postpartum contraceptive use and unmet need for family planning in five low-income countries
Read this article at
Abstract
Background
During the post-partum period, most women wish to delay or prevent future pregnancies. Despite this, the unmet need for family planning up to a year after delivery is higher than at any other time. This study aims to assess fertility intention, contraceptive usage and unmet need for family planning amongst women who are six weeks postpartum, as well as to identify those at greatest risk of having an unmet need for family planning during this period.
Methods
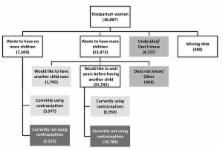
Using the NICHD Global Network for Women’s and Children’s Health Research’s multi-site, prospective, ongoing, active surveillance system to track pregnancies and births in 100 rural geographic clusters in 5 countries (India, Pakistan, Zambia, Kenya and Guatemala), we assessed fertility intention and contraceptive usage at day 42 post-partum.
Results
We gathered data on 36,687 women in the post-partum period. Less than 5% of these women wished to have another pregnancy within the year. Despite this, rates of modern contraceptive usage varied widely and unmet need ranged from 25% to 96%. Even amongst users of modern contraceptives, the uptake of the most effective long-acting reversible contraceptives (intrauterine devices) was low. Women of age less than 20 years, parity of two or less, limited education and those who deliver at home were at highest risk for having unmet need.
Conclusions
Six weeks postpartum, almost all women wish to delay or prevent a future pregnancy. Even in sites where early contraceptive adoption is common, there is substantial unmet need for family planning. This is consistently highest amongst women below the age of 20 years. Interventions aimed at increasing the adoption of effective contraceptive methods are urgently needed in the majority of sites in order to reduce unmet need and to improve both maternal and infant outcomes, especially amongst young women.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Family planning: the unfinished agenda.
- Record: found
- Abstract: found
- Article: not found
Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys.
- Record: found
- Abstract: found
- Article: not found