- Record: found
- Abstract: found
- Article: found
Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile
Read this article at
Abstract
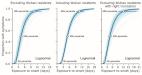
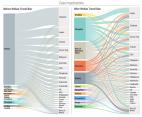
The current COVID-19 pandemic has impacted cities particularly hard. Here, we provide an in-depth characterization of disease incidence and mortality, and their dependence on demographic and socioeconomic strata in Santiago, a highly segregated city and the capital of Chile. Our analyses show a strong association between socioeconomic status and both COVID-19 outcomes and public health capacity. People living in municipalities with low socioeconomic status did not reduce their mobility during lockdowns as much as those in more affluent municipalities. Testing volumes may have been insufficient early in the pandemic in those places, and both test positivity rates and testing delays were much higher. We find a strong association between socioeconomic status and mortality, measured either by COVID-19 attributed deaths or excess deaths. Finally, we show that infection fatality rates in young people are higher in low-income municipalities. Together, these results highlight the critical consequences of socioeconomic inequalities on health outcomes.
Related collections
Most cited references43
- Record: found
- Abstract: found
- Article: found
The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak

- Record: found
- Abstract: found
- Article: found