- Record: found
- Abstract: found
- Article: not found
Predicting Outcome after Traumatic Brain Injury: Development and International Validation of Prognostic Scores Based on Admission Characteristics
Read this article at
- oa journal (via doaj)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH title and first author match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via pmcid lookup)
- oa repository (via OAI-PMH doi match)
Powered by 
Abstract
Background
Traumatic brain injury (TBI) is a leading cause of death and disability. A reliable prediction of outcome on admission is of great clinical relevance. We aimed to develop prognostic models with readily available traditional and novel predictors.
Methods and Findings
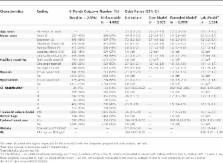
Prospectively collected individual patient data were analyzed from 11 studies. We considered predictors available at admission in logistic regression models to predict mortality and unfavorable outcome according to the Glasgow Outcome Scale at 6 mo after injury. Prognostic models were developed in 8,509 patients with severe or moderate TBI, with cross-validation by omission of each of the 11 studies in turn. External validation was on 6,681 patients from the recent Medical Research Council Corticosteroid Randomisation after Significant Head Injury (MRC CRASH) trial. We found that the strongest predictors of outcome were age, motor score, pupillary reactivity, and CT characteristics, including the presence of traumatic subarachnoid hemorrhage. A prognostic model that combined age, motor score, and pupillary reactivity had an area under the receiver operating characteristic curve (AUC) between 0.66 and 0.84 at cross-validation. This performance could be improved (AUC increased by approximately 0.05) by considering CT characteristics, secondary insults (hypotension and hypoxia), and laboratory parameters (glucose and hemoglobin). External validation confirmed that the discriminative ability of the model was adequate (AUC 0.80). Outcomes were systematically worse than predicted, but less so in 1,588 patients who were from high-income countries in the CRASH trial.
Conclusions
Prognostic models using baseline characteristics provide adequate discrimination between patients with good and poor 6 mo outcomes after TBI, especially if CT and laboratory findings are considered in addition to traditional predictors. The model predictions may support clinical practice and research, including the design and analysis of randomized controlled trials.
Abstract
Ewout Steyerberg and colleagues describe a prognostic model for the prediction of outcome of traumatic brain injury using data available on admission.
Editors' Summary
Background.
Traumatic brain injury (TBI) causes a large amount of morbidity and mortality worldwide. According to the Centers for Disease Control, for example, about 1.4 million Americans will sustain a TBI—a head injury—each year. Of these, 1.1 million will be treated and released from an emergency department, 235,000 will be hospitalized, and 50,000 will die. The burden of disease is much higher in the developing world, where the causes of TBI such as traffic accidents occur at higher rates and treatment may be less available.
Why Was This Study Done?
Given the resources required to treat TBI, a very useful research tool would be the ability to accurately predict on admission to hospital what the outcome of a given injury might be. Currently, scores such as the Glasgow Coma Scale are useful to predict outcome 24 h after the injury but not before.
Prognostic models are useful for several reasons. Clinically, they help doctors and patients make decisions about treatment. They are also useful in research studies that compare outcomes in different groups of patients and when planning randomized controlled trials. The study presented here is one of a number of analyses done by the IMPACT research group over the past several years using a large database that includes data from eight randomized controlled trials and three observational studies conducted between 1984 and 1997. There are other ongoing studies that also seek to develop new prognostic models; one such recent study was published in BMJ by a group involving the lead author of the PLoS Medicine paper described here.
What Did the Researchers Do and Find?
The authors analyzed data that had been collected prospectively on individual patients from the 11 studies included in the database and derived models to predict mortality and unfavorable outcome at 6 mo after injury for the 8,509 patients with severe or moderate TBI. They found that the strongest predictors of outcome were age, motor score, pupillary reactivity, and characteristics on the CT scan, including the presence of traumatic subarachnoid hemorrhage. A core prognostic model could be derived from the combination of age, motor score, and pupillary reactivity. A better score could be obtained by adding CT characteristics, secondary problems (hypotension and hypoxia), and laboratory measurements of glucose and hemoglobin. The scores were then tested to see how well they predicted outcome in a different group of patients—6,681 patients from the recent Medical Research Council Corticosteroid Randomisation after Significant Head Injury (MRC CRASH) trial.
What Do These Findings Mean?
In this paper the authors show that it is possible to produce prognostic models using characteristics collected on admission as part of routine care that can discriminate between patients with good and poor outcomes 6 mo after TBI, especially if the results from CT scans and laboratory findings are added to basic models. This paper has to be considered together with other studies, especially the paper mentioned above, which was recently published in the BMJ ( MRC CRASH Trial Collaborators [2008] Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ 336: 425–429. ). The BMJ study presented a set of similar, but subtly different models, with specific focus on patients in developing countries; in that case, the patients in the CRASH trial were used to produce the models, and the patients in the IMPACT database were used to verify one variant of the models. Unfortunately this related paper was not disclosed to us during the initial review process; however, during PLoS Medicine's subsequent consideration of this manuscript we learned of it. After discussion with the reviewers, we took the decision that the models described in the PLoS Medicine paper are sufficiently different from those reported in the other paper and as such proceeded with publication of the paper. Ideally, however, these two sets of models would have been reviewed and published side by side, so that readers could easily evaluate the respective merits and value of the two different sets of models in the light of each other. The two sets of models are, however, discussed in a Perspective article also published in PLoS Medicine (see below).
Additional Information.
Please access these Web sites via the online version of this summary at http://dx.doi.org/10.1371/journal.pmed.0050165.
-
This paper and the BMJ paper mentioned above are discussed further in a PLoS Medicine Perspective article by Andrews and Young
-
The TBI Impact site provides a tool to calculate the scores described in this paper
-
The CRASH trial, which is used to validate the scores mentioned here, has a Web site explaining the trial and its results
-
The R software, which was used for the prognostic analyses, is freely available
-
The MedlinePlus encyclopedia has information on head injury
-
The WHO site on neurotrauma discusses head injury from a global perspective
-
The CDC's National Center for Injury Prevention and Control gives statistics on head injury in the US and advice on prevention
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Missing data: our view of the state of the art.
- Record: found
- Abstract: not found
- Book: not found