- Record: found
- Abstract: found
- Article: found
Multiple Fentanyl Overdoses — New Haven, Connecticut, June 23, 2016
research-article
Anthony J. Tomassoni , MD
1
,
,
Kathryn F. Hawk , MD
1 ,
Karen Jubanyik , MD
1 ,
Daniel P. Nogee , MD
1 ,
Thomas Durant , MD
2 ,
Kara L. Lynch , PhD
3 ,
Rushaben Patel , PharmD
2 ,
David Dinh , PharmD
2 ,
Andrew Ulrich , MD
1 ,
Gail D’Onofrio , MD
1
03 February 2017
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
On the evening of June 23, 2016, a white powder advertised as cocaine was purchased
off the streets from multiple sources and used by an unknown number of persons in
New Haven, Connecticut. During a period of less than 8 hours, 12 patients were brought
to the emergency department (ED) at Yale New Haven Hospital, experiencing signs and
symptoms consistent with opioid overdose. The route of intoxication was not known,
but presumed to be insufflation (“snorting”) in most cases. Some patients required
doses of the opioid antidote naloxone exceeding 4 mg (usual initial dose = 0.1–0.2
mg intravenously), and several patients who were alert after receiving naloxone subsequently
developed respiratory failure. Nine patients were admitted to the hospital, including
four to the intensive care unit (ICU); three required endotracheal intubation, and
one required continuous naloxone infusion. Three patients died. The white powder was
determined to be fentanyl, a drug 50 times more potent than heroin, and it included
trace amounts of cocaine. The episode triggered rapid notification of public health
and law enforcement agencies, interviews of patients and their family members to trace
and limit further use or distribution of the fentanyl, immediate naloxone resupply
and augmentation for emergency medical services (EMS) crews, public health alerts,
and plans to accelerate naloxone distribution to opioid users and their friends and
families. Effective communication and timely, coordinated, collaborative actions of
community partners reduced the harm caused by this event and prevented potential subsequent
episodes.
Shortly after 4:00 p.m. on June 23, 2016, four patients with symptoms and signs of
opioid overdose, characterized by central nervous system and respiratory depression,
miosis (pinpoint pupil constriction), hypotension, and bradycardia, arrived in rapid
succession at the York Street Campus (two patients) and St. Raphael Campus (two patients)
EDs of Yale New Haven Hospital in downtown New Haven. Within 6 hours, seven additional
patients arrived at the York Street Campus ED and one more at the St. Raphael ED;
these patients included two who were pronounced dead on arrival and four critically
ill patients requiring endotracheal intubation and ICU admission (Figure). The patients
represented four geographic clusters (i.e., at least one other victim found in the
same vehicle or parking lot, or in the same house or an adjacent house), and were
transported by EMS crews responding to bystander 911 calls. All of the patients had
clinical signs of opioid overdose and received at least one dose of naloxone from
EMS (Table 1). Twelve patients met the case definition for suspected fentanyl exposure
(i.e., clinical signs of opioid toxicity and response to naloxone, with laboratory
confirmation of fentanyl or fentanyl metabolites in blood, or history of direct association
with a laboratory-confirmed fentanyl exposure) (Table 1). Among the four patients
admitted to the ICU, three required endotracheal intubation and mechanical ventilation
for respiratory failure that was relatively refractory to large doses of naloxone,
and one required a continuous naloxone infusion for 12 hours. Two of the three intubated
patients suffered acute kidney injury and pulmonary or gastrointestinal hemorrhage,
one of whom (patient K) died 3 days later from multisystem organ failure. The third
patient survived with permanent cardiac injury. Other intoxicated patients who arrived
at the ED with signs or symptoms of the opioid toxidrome were excluded from this analysis
because of inconsistent history (e.g., patient reported using a nonfentanyl opioid)
or toxicology test results that did not identify fentanyl.
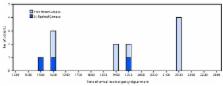
FIGURE
Time of arrival for 12 fentanyl overdose patients at the St. Raphael Campus (n = 3)
and York Street Campus (n = 9) emergency departments of Yale New Haven Hospital —
New Haven, Connecticut, June 23, 2016
The figure above is a bar chart showing the time of arrival for 12 fentanyl overdose
patients at the St. Raphael Campus (n = 3) and York Street Campus (n = 9) emergency
departments of Yale New Haven Hospital in New Haven, Connecticut on June 23, 2016.
TABLE 1
Demographic characteristics, hospital arrival time, prehospital naloxone use, and
disposition for 12 patients with fentanyl overdose — Yale New Haven Hospital, New
Haven, Connecticut, June 23, 2016
Patient
Age group (decade)
Sex
Arrival time
Emergency department
Naloxone(Administering provider, route)
Disposition
(EMS, IN)
(EMS, IV/IO)
(ED/IV)
A
60s
Male
16:16
SRC
2 mg
0
0
Discharged
B
80s
Male
16:36
YSC
2 mg
1 mg
0
Observed and discharged
C
30s
Male
16:40
YSC
3 mg
0
0.4 mg
Intensive care unit
D
40s
Male
16:48
SRC
3 mg
0
0.4 mg
Observed and discharged
E
70s
Male
19:01
YSC
4 mg
2 mg*
0
Dead on arrival in ED
F
70s
Male
19:16
YSC
2 mg
2 mg
2 mg
Observed and discharged
G
60s
Male
19:33
YSC
2 mg
2 mg
0.4 mg
Observed and discharged
H
60s
Male
19:38
SRC
2 mg
2 mg
0.4 mg†
Intensive care unit
I
30s
Female
21:31
YSC
0
2 mg
2 mg
Dead on arrival in ED
J
50s
Female
21:32
YSC
2 mg
1 mg
0
Intensive care unit
K
60s
Male
21:39
YSC
0
0.5 mg
0
Intensive care unit§
L
50s
Female
21:41
YSC
2 mg
2 mg
0
Observed and discharged
Abbreviations: ED = emergency department; EMS = emergency medical services; IN = intranasal;
IO = intraosseous; IV = intravenous; SRC = St. Raphael Campus; YSC = York Street Campus.
* Intraosseous injection.
† Naloxone drip 0.4 mg/hour for 12 hours in intensive care unit.
§ Patient died of multiorgan failure in intensive care unit 3 days later.
Shortly after arrival in the ED, serum toxicology screens, designed to detect a panel
of nonopioid toxins, were performed for all patients, and qualitative urine immunoassay
toxicology screens for drugs of abuse were performed for nine patients (A, C, D, F,
G, H, J, K, and L) (Table 2). The urine immunoassay screening tests cannot detect
fentanyl and its analogs; however, all but one of the nine tested positive for cocaine.
The one patient with a negative urine cocaine screen (patient A) acknowledged past
cocaine use. Serum and urine specimens were later analyzed at the University of California,
San Francisco (UCSF) using liquid chromatography high-resolution mass spectrometry
(LC-HRMS) (
1
) to detect 215 common illicit and pharmaceutical drugs and metabolites, followed
by additional analyses in attempts to identify 7,038 novel drugs and metabolites (
2
,
3
). Levels of fentanyl, cocaine, benzoylecgonine (a cocaine metabolite that persists
in body fluids and is an indicator of cocaine use) and levamisole (a veterinary antihelminthic
that has been used as a cocaine adulterant) were quantified. Nine patients (B, C,
D, F, G, H, J, K, and L) had fentanyl detected in blood that was collected during
their hospitalization and tested at UCSF (Table 2). One patient who reported cocaine
use before symptom onset (patient A) and who was found in the vicinity of patients
B, C, and D at the time of intoxication, was discharged before the full scope of the
outbreak had been recognized and did not receive confirmatory toxicology testing.
The Connecticut Medical Examiner’s Office performed postmortem toxicology screens
on specimens obtained from two patients who died en route to the hospital (patients
E and I).
TABLE 2
Serum and urine toxicology test results for 12 patients with fentanyl overdose — Yale
New Haven Hospital, New Haven, Connecticut, June 23, 2016
Patient
Serum levels (ng/mL)
Other substances detected
Fentanyl
Cocaine
BE
Levamisole
Serum
Urine
A
—*
—
—
—
—
—
B
0.9
Not detected
1
1
BE, cotinine, levamisole, norfentanyl
Specimen not available
C
0.5
0
65
13
BE, cotinine, levamisole, norfentanyl, THC-COOH
BE, cocaethylene, cocaine, cotinine, EME, levamisole, lidocaine, naloxone, nicotine,
norcocaine, norfentanyl
D
0.6
0
1
1
BE, cotinine, levamisole, norfentanyl, THC-COOH
BE, cocaethylene, cocaine, EME, ethylone, hydrocodone, levamisole, naloxone, norfentanyl,
THC-COOH
E†
11
Not detected
Not detected
—
Ethanol
—
F
4.6
2
15
2
BE, cocaethylene, cocaine, cotinine, hydroxyzine, levamisole, naloxone, norfentanyl
BE, EME, cocaethylene, cocaine, cotinine, hydroxyzine, levamisole, naloxone, norfentanyl
G
2.3
1
63
4
Acetaminophen, BE, cocaine, cotinine, levamisole, midazolam, norfentanyl, THC-COOH
α-hydroxymidazolan, acetaminophen, BE, cocaine, cotinine, EME, levamisole, midazolam,
naloxone, norcocaine, norfentanyl
H
1.9
26
144
5
Acetaminophen, BE, cocaethylene, cocaine, cotinine, levamisole, naloxone, norfentanyl
Acetaminophen, BE, cocaine, cotinine, EME, hydroxyzine, levamisole, naloxone, nicotine,
norcocaine, norfentanyl
I†
13
79
680
—
Cocaethylene, ethanol
—
J
3
26
68
6
BE, cocaine, cotinine, levamisole, naloxone, norfentanyl, tramadol
BE, cocaine, cotinine, EME, desmethyltramadol, levamisole, naloxone, norcocaine, norfentanyl,
tramadol
K§
9.5
3
172
2
BE, cocaine, levamisole, naloxone, norfentanyl, THC-COOH
BE, cocaine, EME, levamisole, norcocaine, norfentanyl
L
3.6
4
712
64
BE, cocaethylene, cocaine, cotinine, hydroxyzine, levamisole, lidocaine, naloxone,
norfentanyl
BE, cocaethylene, cocaine, cotinine, EME, hydroxyzine, levamisole, lidocaine, naloxone,
norfentanyl
Abbreviations: BE = benzoylecgonine; EME = ecgonine methylester; THC-COOH = 11-nor-9-carboxy-
tetrahydrocannabinol.
*Test not performed.
† Postmortem specimens collected by medical examiner.
§ Died in intensive care unit.
Serum samples from the hospitalized patients analyzed at UCSF demonstrated fentanyl
levels of 0.5–9.5 ng/mL (Table 2) (therapeutic range for analgesia = 0.6–3.0 ng/mL)
(
4
); postmortem levels in the first two patients who died were 11 ng/mL (patient E)
and 13 ng/mL (patient I). Norfentanyl, a major metabolite of fentanyl, was detected
in the serum of nine patients; norfentanyl was not detected in postmortem testing
of patients E and I, presumably because death occurred before metabolism of fentanyl
to norfentanyl. All hospitalized patients had detectable serum levels of cocaine,
cocaine metabolites (benzoylecgonine and ecgonine methyl ester), cocaethylene (a compound
formed in vivo when ethanol is ingested in the presence of cocaine), or levamisole
by LC-HRMS confirmatory testing (Table 2), all suggesting recent cocaine use. The
absence of other opioids, such as heroin, methadone, or oxycodone, in serum (only
one patient [D] was hydrocodone positive) was consistent with reports by the patients
that most were not habitual opioid users.
Additional substances detected in serum and urine were reported qualitatively (Table
2) and reflected nicotine (cotinine), cannabinoid (tetrahydrocannabinol), and hydroxyzine
(antihistamine) use, or receipt of naloxone. Postmortem toxicology screens identified
fentanyl as a cause of death for patients E and I, both of whom arrived in the ED
in cardiac arrest. In addition to the clinical specimens, one 32-mg forensic sample
of the illicit drug material collected by law enforcement was tested at the Drug Enforcement
Administration laboratory. Analysis of that product recovered from an involved crime
scene found 6.6% (± 0.8%) fentanyl by weight with trace amounts of cocaine and an
inert adulterant.
Within a few hours of recognition of the outbreak, a multiagency response involving
the New Haven Office of Emergency Management, New Haven and Connecticut Departments
of Public Health, the Drug Enforcement Administration, local police, Connecticut Poison
Control Center, and the New Haven Mayor’s Office was undertaken. Initial actions included
1) rapid notification of public health and law enforcement agencies by ED and EMS
personnel; 2) real-time interviews of patients and family members in an attempt to
trace and limit further use or distribution of the fentanyl; 3) advice to EMS crews
to increase naloxone doses in treating suspected cases; 4) public health alerts regarding
the event, including notices of the sale of a high potency opioid marketed as cocaine
causing deaths in the region; and 5) plans to accelerate distribution of naloxone
to opioid users and their friends and families. The high naloxone requirements necessitated
both immediate naloxone resupply and augmentation for local EMS crews, including the
transfer of 700 naloxone kits from the Connecticut Department of Public Health to
hospitals and EMS crews the following morning. Actions of multiple partners led to
the arrest 4 days later of three persons allegedly responsible for the illicit fentanyl
sales.
Discussion
This explosive occurrence of multiple fentanyl overdoses triggered a rapid response
by public safety and medical communities to identify the substance and its source.
Federal, state, and local agencies responded to confine the outbreak quickly, save
patient lives where possible, alert the public, and gather additional information.
The rapid medical, law enforcement, and public health actions likely limited the extent
and impact of this outbreak.
These events highlight the intrinsic risks inherent in illicit drug use and support
the broad distribution of naloxone. The urine toxicology screens suggest that most
patients were cocaine users, but not chronic opioid users, and as such, would likely
not have received any training in the identification or treatment of opioid overdose.
This episode resulted in the formation of a partnership between the Connecticut Department
of Public Health and Yale New Haven Hospital that facilitated implementation of a
pilot program to provide overdose education and take-home naloxone kits to ED patients
at risk for overdose. In addition, community opioid treatment programs and providers
collaborated with the EDs to provide rapid access to treatment for patients with opioid
use disorders.
Commonly available immunoassay toxicology screening tests are unable to detect fentanyl
or its metabolites; the opiate screen is designed to detect codeine, morphine, and
heroin, and with an expanded panel, oxycodone and methadone. Widespread use of toxicology
screens unable to detect fentanyl or its analogs underscores the importance of recognizing
the opioid toxidrome. Rescuers and clinicians should recognize the potential need
to administer multiple or high doses of naloxone in cases of opioid overdose that
do not respond to administration of a single standard naloxone dose where fentanyl
or its analogs (highly potent opioids) might be responsible for unresponsiveness.
The total dose of naloxone required for opioid reversal will depend on many factors,
including the opioid dose, the potency of the opioid in binding receptors, the lipophilicity
of the opioid in crossing into the central nervous system, the elimination half-life
of the opioid, individual patient factors, and the route of administration of the
naloxone (intranasal compared with intramuscular or intravenous) (5–7). Because of
the persistent respiratory depression associated with fentanyl, additional doses of
naloxone might be needed after initial reversal.*
Although illicit opioids often are mixed with harmful adulterants (e.g., fentanyl
and its analogs blended with or deliberately substituted for heroin or mixed with
the opioid analgesic combination of acetaminophen and hydrocodone [e.g., Norco]) (
8
,
9
), this outbreak was unique in representation of fentanyl as cocaine to an opioid-naïve
population, which resulted in an outbreak of fatal and nonfatal overdoses.
Lack of metabolism of fentanyl to norfentanyl might be the result of rapid death after
fentanyl use (
10
). It has been suggested that rapid death might be caused by immediate onset of respiratory
arrest or that fentanyl might cause rapid onset of chest wall rigidity, leading to
death (10). This effect of fentanyl is well recognized by clinicians familiar with
the drug, but is not likely to be known among illicit drug users. In addition, many
users might be unaware that their expected substance of choice might be substituted
by or adulterated with high doses of fentanyl.
Distribution of naloxone to persons at risk for opioid overdose, their families, and
friends through prescriptions by practitioners, pharmacists, and other public health
avenues might help prevent fatal fentanyl overdoses. In addition, this outbreak of
severe opioid intoxication among patients who were cocaine users, but not chronic
opioid users, suggests that distributing naloxone and offering training to all illicit
drug users, their friends, and family members might prevent such opioid-associated
morbidity and mortality. The swift coordinated multiagency response likely limited
the impact of this outbreak, and the resultant strengthening of community partnerships
has the potential to further limit the morbidity and mortality related to opioids
in communities.
Summary
What is already known about this topic?
Fentanyl and its analogs have been substituted for heroin and other opioids, and are
usually marketed to persons seeking opioids. Because of fentanyl’s high potency compared
with heroin, methadone, and oxycodone, there is a high risk for fatal overdose associated
with illicit use. Higher than normal doses of the opioid antagonist naloxone might
be required to reverse fentanyl overdose.
What is added by this report?
On June 23, 2016, fentanyl marketed as cocaine resulted in an extraordinary opioid
overdose outbreak in New Haven, Connecticut, resulting within 6 hours in at least
12 cases, marked by four intensive care unit admissions and three deaths. A rapid
and coordinated public health response involving multiple partners likely reduced
the impact of this outbreak.
What are the implications for public health practice?
A collaborative and timely multi-organization response can mitigate the consequences
of an extraordinary public health event. Development and implementation of a screening
test for fentanyl might inform clinicians about the presence of these particularly
deadly opioids and prevent deaths. Opioid use education and naloxone administration
kits and education should be extended to all persons at risk for illicit drug use,
their families, and friends.
Related collections
Most cited references10
- Record: found
- Abstract: not found
- Article: not found
A review of the use of fentanyl analgesia in the management of acute pain in adults.
- Record: found
- Abstract: found
- Article: not found
Fentanyl epidemic in Chicago, Illinois and surrounding Cook County.
J Denton, Heather Schumann, Tim Erickson … (2008)
- Record: found
- Abstract: found
- Article: not found
Reducing the harm of opioid overdose with the safe use of naloxone : a pharmacologic review.
Hong K Kim, Lewis Nelson (2015)