- Record: found
- Abstract: found
- Article: found
Use of an electronic administrative database to identify older community dwelling adults at high-risk for hospitalization or emergency department visits: The elders risk assessment index
Read this article at
Abstract
Background
The prevention of recurrent hospitalizations in the frail elderly requires the implementation of high-intensity interventions such as case management. In order to be practically and financially sustainable, these programs require a method of identifying those patients most at risk for hospitalization, and therefore most likely to benefit from an intervention. The goal of this study is to demonstrate the use of an electronic medical record to create an administrative index which is able to risk-stratify this heterogeneous population.
Methods
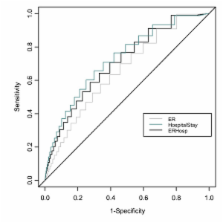
We conducted a retrospective cohort study at a single tertiary care facility in Rochester, Minnesota. Patients included all 12,650 community-dwelling adults age 60 and older assigned to a primary care internal medicine provider on January 1, 2005. Patient risk factors over the previous two years, including demographic characteristics, comorbid diseases, and hospitalizations, were evaluated for significance in a logistic regression model. The primary outcome was the total number of emergency room visits and hospitalizations in the subsequent two years. Risk factors were assigned a score based on their regression coefficient estimate and a total risk score created. This score was evaluated for sensitivity and specificity.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: not found
Geriatric care management for low-income seniors: a randomized controlled trial.
- Record: found
- Abstract: found
- Article: not found
A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department--the DEED II study.
- Record: found
- Abstract: found
- Article: not found