- Record: found
- Abstract: found
- Article: found
Abridged version of the AWMF guideline for the medical clinical diagnostics of indoor mould exposure : S2K Guideline of the German Society of Hygiene, Environmental Medicine and Preventive Medicine (GHUP) in collaboration with the German Association of Allergists (AeDA), the German Society of Dermatology (DDG), the German Society for Allergology and Clinical Immunology (DGAKI), the German Society for Occupational and Environmental Medicine (DGAUM), the German Society for Hospital Hygiene (DGKH), the German Society for Pneumology and Respiratory Medicine (DGP), the German Mycological Society (DMykG), the Society for Pediatric Allergology and Environmental Medicine (GPA), the German Federal Association of Pediatric Pneumology (BAPP), and the Austrian Society for Medical Mycology (ÖGMM)
Read this article at
Abstract
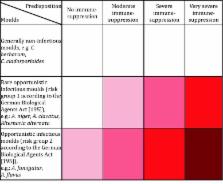
This article is an abridged version of the AWMF mould guideline “Medical clinical diagnostics of indoor mould exposure” presented in April 2016 by the German Society of Hygiene, Environmental Medicine and Preventive Medicine ( Gesellschaft für Hygiene, Umweltmedizin und Präventivmedizin, GHUP), in collaboration with the above-mentioned scientific medical societies, German and Austrian societies, medical associations and experts. Indoor mould growth is a potential health risk, even if a quantitative and/or causal relationship between the occurrence of individual mould species and health problems has yet to be established. Apart from allergic bronchopulmonary aspergillosis (ABPA) and mould-caused mycoses, only sufficient evidence for an association between moisture/mould damage and the following health effects has been established: allergic respiratory disease, asthma (manifestation, progression and exacerbation), allergic rhinitis, hypersensitivity pneumonitis (extrinsic allergic alveolitis), and increased likelihood of respiratory infections/bronchitis. In this context the sensitizing potential of moulds is obviously low compared to other environmental allergens. Recent studies show a comparatively low sensitizing prevalence of 3–10% in the general population across Europe. Limited or suspected evidence for an association exist with respect to mucous membrane irritation and atopic eczema (manifestation, progression and exacerbation). Inadequate or insufficient evidence for an association exist for chronic obstructive pulmonary disease, acute idiopathic pulmonary hemorrhage in children, rheumatism/arthritis, sarcoidosis and cancer. The risk of infection posed by moulds regularly occurring indoors is low for healthy persons; most species are in risk group 1 and a few in risk group 2 ( Aspergillus fumigatus, A. flavus) of the German Biological Agents Act ( Biostoffverordnung). Only moulds that are potentially able to form toxins can be triggers of toxic reactions. Whether or not toxin formation occurs in individual cases is determined by environmental and growth conditions, above all the substrate. In the case of indoor moisture/mould damage, everyone can be affected by odour effects and/or mood disorders. However, this is not a health hazard. Predisposing factors for odour effects can include genetic and hormonal influences, imprinting, context and adaptation effects. Predisposing factors for mood disorders may include environmental concerns, anxiety, condition, and attribution, as well as various diseases. Risk groups to be protected particularly with regard to an infection risk are persons on immunosuppression according to the classification of the German Commission for Hospital Hygiene and Infection Prevention ( Kommission für Krankenhaushygiene und Infektionsprävention, KRINKO) at the Robert Koch- Institute (RKI) and persons with cystic fibrosis (mucoviscidosis); with regard to an allergic risk, persons with cystic fibrosis (mucoviscidosis) and patients with bronchial asthma should be protected.
The rational diagnostics include the medical history, physical examination, and conventional allergy diagnostics including provocation tests if necessary; sometimes cellular test systems are indicated. In the case of mould infections the reader is referred to the AWMF guideline “Diagnosis and Therapy of Invasive Aspergillus Infections”. With regard to mycotoxins, there are currently no useful and validated test procedures for clinical diagnostics. From a preventive medicine standpoint it is important that indoor mould infestation in relevant dimension cannot be tolerated for precautionary reasons. With regard to evaluating the extent of damage and selecting a remedial procedure, the reader is referred to the revised version of the mould guideline issued by the German Federal Environment Agency ( Umweltbundesamt, UBA).
Related collections
Most cited references233
- Record: found
- Abstract: found
- Article: not found
EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists
- Record: found
- Abstract: found
- Article: not found
Aspergillus fumigatus and aspergillosis.
- Record: found
- Abstract: found
- Article: found